题目:妊娠早期血小板减少症可预测产科抗磷脂综合征的不良妊娠结局
期刊:Frontiers in Immunology
发表时间:2022年8月
关键词:抗磷脂综合征,早产,小于胎龄儿,血小板减少,宫内胎儿死亡
摘要翻译
背景:血小板减少是抗磷脂综合征(APS)的常见表现,也是使用了低剂量阿司匹林(LDA)和低分子肝素(LMWH)的产科APS(OAPS)标准治疗中出血的主要原因。
目的:本研究评估OAPS患者妊娠早期血小板减少与不良妊娠结局(APO)之间的可能关系。
方法:在北京大学人民医院进行了一项病例对照研究。收集OAPS患者的临床、免疫学和妊娠结局。应用单因素和多因素logistic回归分析评估妊娠早期血小板减少与APO之间的关系。
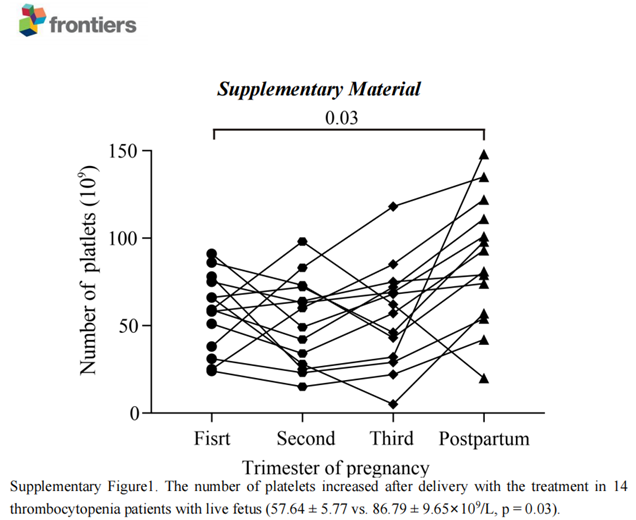
结果:共有115名参与者被纳入分析。两组在产前、产后出血方面无明显差异。血小板减少组胎龄小于对照组(34.12±8.44 vs 37.44士3.81)周,差异有统计学意义(P=0.023)。低补体血症、抗磷脂抗体双阳以及存在高滴度β2糖蛋白1和/或抗心磷脂抗体的APS患者会更容易出现血小板减少(P<0.05)。与对照组相比,妊娠早期血小板减少与小于胎龄儿 (12.12% vs 31.25%,P=0.043)、早产(<37周) (16.16% vs 43.75%,p=0.010)和宫内胎儿死亡(2.02% vs 12.50%,p=0.033) 相关。在调整人口统计学和实验室因素后,妊娠早期血小板减少是早产的独立危险因素(OR=5.40,95%CI:1.35-21.53,p=0.02)。加上药物调整之后,上述因素无显著性差异(P>0.05)。值得注意的是,有活胎的14例血小板减少症患者分娩后血小板数量增加(p=0.03)。
结论:这项研究表明,妊娠早期血小板减少会增加APS患者早产的风险,有效的OAPS治疗可改善妊娠结局,且不增加产前、产后出血的风险。
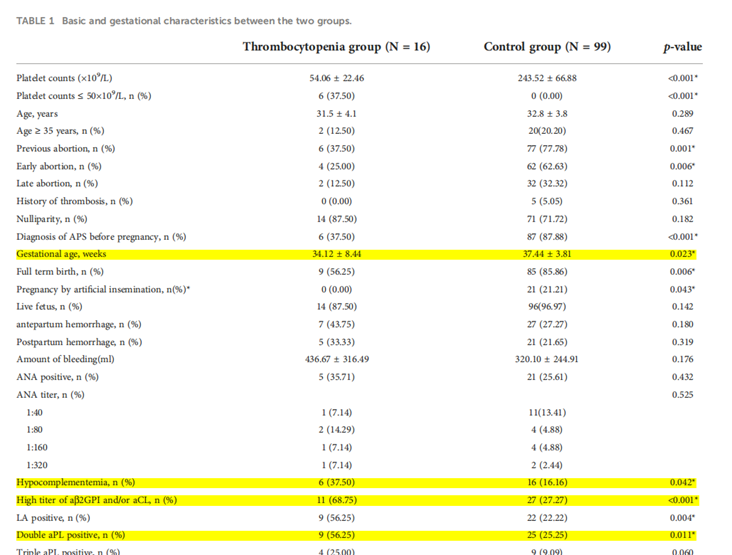
基础信息表
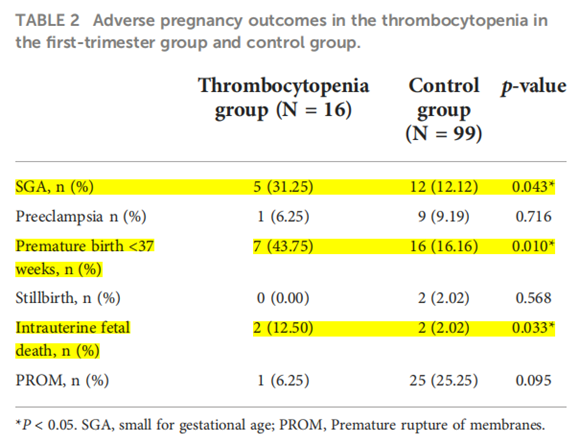
血小板减少症患者组与对照组对比
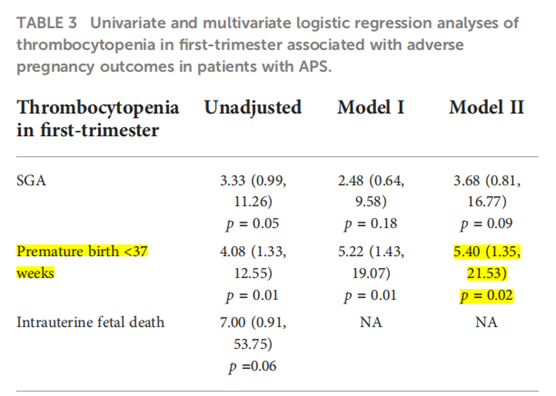
单因素与多因素逻辑回归分析APS患者妊娠早期不良妊娠结局事件
原文
Background: Thrombocytopenia is a common manifestation of antiphospholipid syndrome (APS), and is a main concern for bleeding on the standard treatment of low dose aspirin (LDA) and low molecular weight heparin (LMWH) in obstetric APS (OAPS).
Objective: This study assesses the possible relationship between thrombocytopenia during the first trimester and adverse pregnancy outcomes (APOs) in OAPS patients.
Methods: A case-control study was conducted at Peking University People’s Hospital, Beijing, China. The clinical, immunologic, and pregnancy outcomes of the OAPS patients were collected. Univariate and multivariate logistic regression analyses were applied to assess the relationship between APOs and thrombocytopenia in the first trimester.
Results: A total of 115 participants were included in the analysis. There were no difference on antepartum and postpartum hemorrhage between the two groups. The gestational age in the thrombocytopenia group was less than that in the control group (34.12±8.44 vs 37.44±3.81 weeks, p=0.023). Hypocomplementemia, double aPL positive, and high titers of anti-b2 glycoprotein I were more frequent in APS patients with thrombocytopenia (p<0.05). Compared to the control group, thrombocytopenia in the first trimester was correlated with SGA (12.12% vs 31.25%, p=0.043), premature birth <37 weeks (16.16% vs 43.75%, p = 0.010) and intrauterine fetal death (2.02% vs 12.50%, p=0.033). Thrombocytopenia in first-trimester independently increased the risk of preterm birth<37weeks (OR=5.40, 95% CI: 1.35-21.53, p=0.02) after adjusting for demographic and laboratory factors. After adding medication adjustments, these factors above become insignificant (p>0.05). Of note, the number of platelets increased after delivery in 14 thrombocytopenia patients with live fetuses (p=0.03).
Conclusion: This study demonstrates that thrombocytopenia in the first trimester increases the risks of preterm birth in women with APS. The effective OAPS treatments may improve pregnancy outcomes and not increase the risk of antepartum and postpartum hemorrhage.
参考文献:Jin J, Xu X, Hou L, Hou Y, Li J, Liang M, Li C. Thrombocytopenia in the first trimester predicts adverse pregnancy outcomes in obstetric antiphospholipid syndrome. Front Immunol. 2022 Aug 18;13:971005.